http://https://www.youtube.com/watch?v=lOi23FuGmr4&feature=emb_logo
At USAHS, we have a student-first philosophy, which means flexible learning, innovative curricula and career-focused practice. With access to state-of-the-art simulation labs and expert faculty we stay ahead of the competition by providing our students—early on in their program—the opportunity for hands-on practice with the tools and technology they need to stand out from the rest and be practice-ready after graduation.
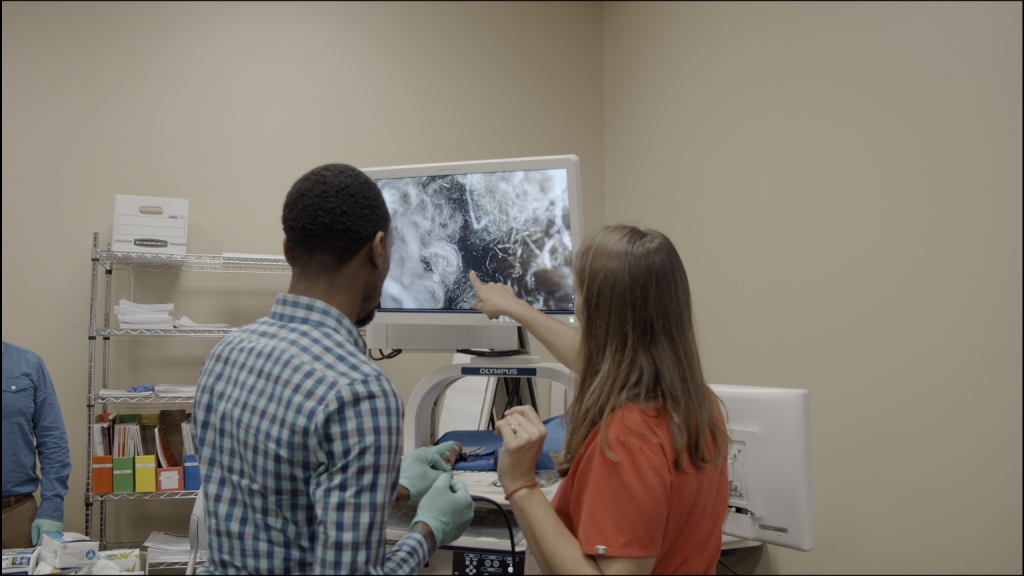
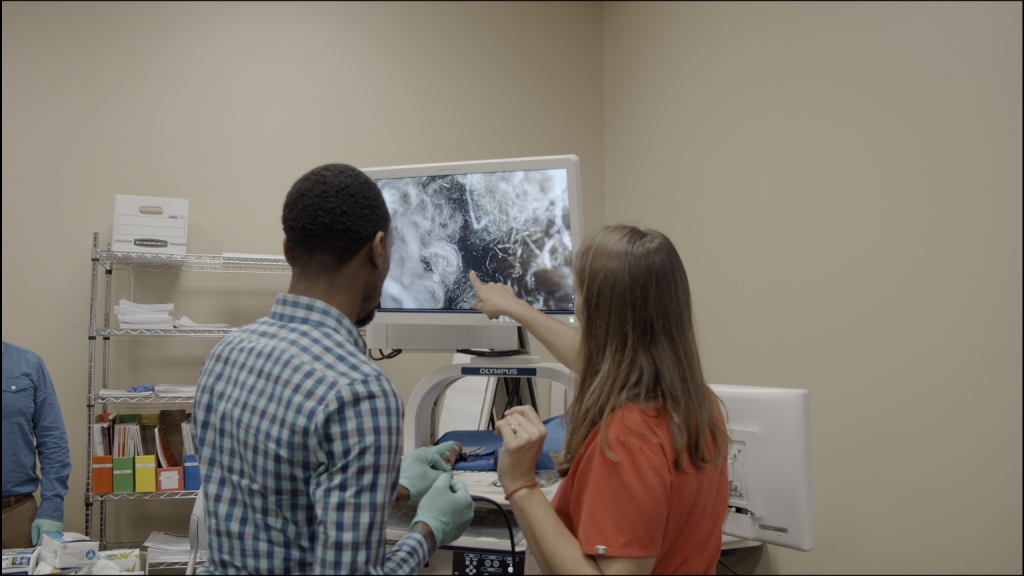
Because of our student-first approach, we have recently incorporated our advanced endoscopy equipment for the clinical simulation centers on our Austin and Dallas campuses. Students in our Master of Science in Speech-Language Pathology (MS-SLP) program practice using two different types of endoscopes in a clinical setting.
Both campuses are equipped with two rigid oral endoscopes and two flexible nasopharyngoscopes manufactured by Olympus, known for making lenses and cameras. Our MS-SLP students use these instruments during the on-campus clinical immersions in their third and fifth trimesters.
Assessing Vocal Fold Pathologies
The oral endoscope is a rigid scope that practitioners place in the patient’s mouth to perform a videostroboscopy, an evaluation to assess vocal fold dynamics. Physicians who are ear, nose, and throat (ENT) specialists use both rigid and flexible endoscopes to diagnose vocal fold pathologies, such as nodules, cysts, polyps, and hemorrhages. Working in collaboration with the ENT, a speech-language pathologist (SLP) diagnoses dysphonia, or voice disorders (including hoarse, breathy, harsh, or rough vocal qualities), caused by those pathologies.
In the USAHS simulation labs, students practice placing the rigid scope correctly in each other’s mouths while holding the tongue down with gauze. The instrument can elicit the gag reflex in sensitive people; when this happens, it helps for the patient to suck the scope in like a straw as the endoscopist slowly moves the oral endoscope toward the oropharynx to view the vocal folds. There is a 70-degree angle on the scope that allows for a clear view of the larynx and vocal folds once this point is reached. A digital image of the patient’s vocal folds is visible on a large screen.
Our labs also have stroboscopies (an instrument emitting a strobe light), which allow students to see the perceived motion of vocal folds in real time and assess a patient’s vocal folds for symmetry, amplitude, periodicity, mucosal wave, and glottal closure.
Visualizing Swallowing Disorders
The nasopharyngoscope is a flexible scope that goes up one nostril and down through the nasal cavity so that practitioners can view the patient’s oropharynx and hypopharyngeal structures. It is within the SLP’s scope of practice to perform videostroboscopies and also fiberoptic endoscopy evaluation of swallowing (FEES), a test to assess dysphagia (difficulty swallowing).
The flexible nasopharyngoscope is used to perform both of the aforementioned evaluations. Students practice navigating the instrument—first by advancing it between the folds of a washcloth, then by going into the nose of a manikin head that has mock vocal folds. Fine motions of a lever control the movement of the lens at the tip, and students can see the vocal folds on a large screen. Once they’ve mastered this technique, students practice on each other.
“Sometimes there’s a student who’s queasy about it,” Hines-Staples says. “But for the most part, they are geared up for this.” Hines-Staples says that today, the flexible scope is much more commonly used than the rigid scope, since the rigid scope is only used to perform videostroboscopies. The rigid scope is used for diagnosing vocal fold pathologies and is also a better choice for patients who have a deviated septum or who are too squeamish about having a scope go into their nose.
Seeing Anatomy in Action
A specialist in dysphagia and voice disorders, Hines-Staples has worked as an SLP for 14 years—primarily in acute care, from NICU through geriatric settings. She has taught students to use this brand-new equipment at four USAHS immersions to date. “They love it,” she says. “It really helps them connect the dots. They learn anatomy in the wet lab, dissecting cadavers—and then they see that anatomy in action.”
During some immersion sessions, USAHS offers a pro bono speech-language pathology clinic in the Austin community. Children and adults come in for speech, voice, language, and hearing evaluations. Hines-Staples says plans are in the works to have students, with faculty oversight, use the endoscopy equipment to practice performing cancer screenings in patients or FEES and videostroboscopies on patients who have a doctor’s order.
“In traditional programs, you don’t usually get this training,” Hines-Staples says. “When they interview for their clinical fellowship, our students can say that they have actual hands-on training in this equipment. It can really set them apart.”
The University of St. Augustine for Health Sciences (USAHS) offers a Master of Science in Speech-Language Pathology (MS-SLP). Designed for working students, the MS-SLP is an online program with four required on-campus residencies on either the USAHS Austin or Dallas campus. The program offers two intakes per year, in January and September. Prepare to make a difference in the lives of clients across the lifespan with a meaningful career in speech therapy!








